ER demand climbs, hospital discharges delayed as pandemic enters its third year
8 min read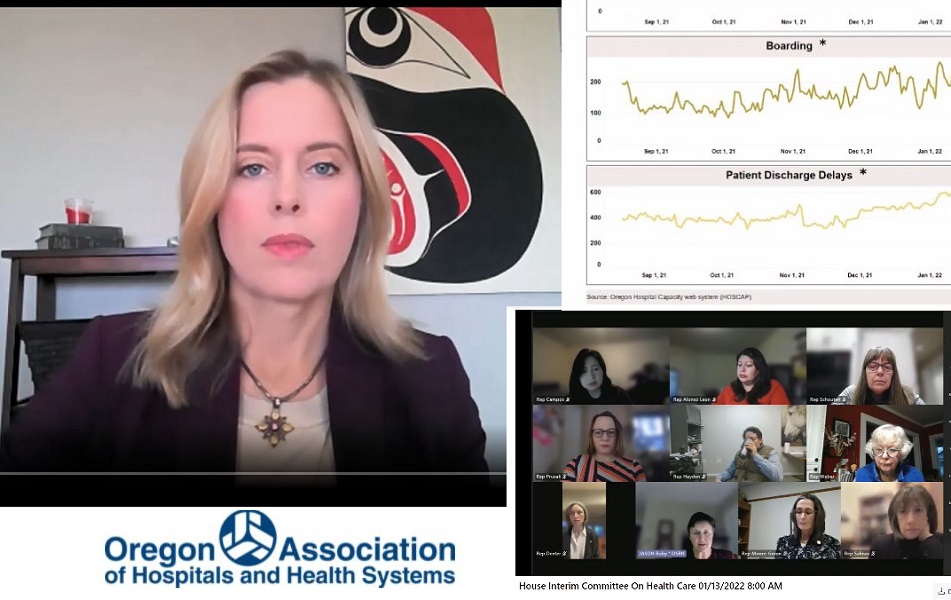
Becky Hultberg and Andi Easton of OAHHS outlined the Omicron variant's impact on Oregon hospitals, and endorsed a legislative package coming up during the short session.
The good news is, Oregonians are getting less sick from the Omicron variant and aren’t filling up the ICUs (intensive care units). The bad news: This surge is affecting emergency rooms and revealing the system’s growing fragility. A press conference on January 20th.
[00:00:15] Dave Northfield: Here is Becky Hultberg, who is the President and CEO of the Oregon Association of Hospitals and Health Systems.
[00:00:22] Becky Hultberg: This Omicron surge is different than Delta. This is putting more pressure on emergency departments and regular medical units, whereas the Delta surge put more pressure on ICUs.
[00:00:32] Omicron is impacting all regions of the state and pretty much all hospitals in the state. The lack of available hospital beds is pushing the system everywhere to a breaking point. There is good news. The good news is that most patients in the hospital with COVID-19 aren’t as sick as they were during the Delta wave, but the sheer number of patients, exacerbated by staffing and discharge challenges has the potential to overwhelm the healthcare system. The next couple of weeks, they’re going to be really tough and it is important for people to understand that. There is a war going on in our hospitals against this virus that isn’t visible to the public.
[00:01:11] John Q: Becky said one big challenge is staffing.
Thank you for supporting
local citizen journalism
[00:01:13] Becky Hultberg: Hospitals are in a much worse position with staffing that at any prior point in the pandemic. You know, after two years on this COVID-19 rollercoaster, many healthcare professionals just want off. Staff are physically and emotionally exhausted and dealing with challenging patients and conditions. Nationally, nearly one in five healthcare workers has quit during the pandemic. So this is not unique to Oregon. Hospitals are also facing significant numbers of staff out sick with COVID-19, just like other organizations. Schools and Oregon businesses have shut down, but that is not an option for a hospital. These staffing shortages are causing hospitals to rely heavily on contract staffing, which is very, very expensive and not sustainable over the long-term. It is essential though until the staffing situation stable.
[00:02:02] John Q: We are also seeing challenges in transitioning patients from hospitals to other health care facilities.
[00:02:08] Becky Hultberg: Patients often must be discharged from hospitals to longterm care or other facilities to continue their recovery. And delays in moving patients to these facilities are adding to hospital capacity challenges. So today hospitals have 582 patients who could be discharged from the hospital, but there’s nowhere for them to go. This means that they’re not in the best care setting for their needs. They may need a nursing home or rehab bed, behavioral health support, or they may not even have a home to go to. So the reasons are complex, but it is past time to address this problem. Hospitals have been sounding alarm bells for the entire pandemic about the challenges of discharging patients. And we need help in moving patients out of the hospital to free up beds for people in the community who need them.
[00:02:54] Related to that is the situation around Emergency Department boarding. Patients are waiting in the Emergency Department for available beds in the community or in the hospital. We have 229 of those patients today. Some of these patients need a behavioral health bed. Others need a medical bed, but the beds just aren’t available. And nobody wants to be waiting in an Emergency Department, which is not the best environment for recovery, but that is the reality for many patients today. And this also impacts the ability of hospital emergency departments to handle the huge influx of really sick patients that they’re seeing.
[00:03:25] John Q: Becky said the system also faces challenges related to supplies.
[00:03:29] Becky Hultberg: In the early days, it was around personal protective equipment, and now it’s around other critical resources. There is a national blood shortage crisis, which is also affecting Oregon hospitals. So I want to encourage people to donate blood. We are also dealing with limitations on the supply of monoclonal antibodies and other therapeutics. Hopefully some of these challenges will resolve over the coming weeks, but these are the things that our hospitals are dealing with in real time.
[00:03:55] Oregon’s hospitals are resilient. Much has been asked of them over the last two years from taking care of COVID-19 patients to leading vaccination efforts and they’ve responded, but the pandemic has taken a significant toll. And the healthcare system today is not the same system we had in 2019. So as we were approached COVID-19 recovery, whenever that comes, it’s going to be really important for policy makers and other stakeholders to recognize the fragility of the healthcare system.
[00:04:23] And I want to emphasize that our goal is not to get into crisis standards of care. So we are going to, our hospitals are focusing on how to distribute patients and resources so we can avoid that scenario.
[00:04:34] There have been differences between urban and rural communities around staffing for a long time. This is pre-pandemic. The question, as I understand it, is specifically related to travelers. There is a huge demand for contract staff right now.
[00:04:50] And those contract staff are going to the places where their agencies can receive the highest reimbursement. So, is that putting some rural facilities at a disadvantage? We have heard that it is harder for rural facilities to secure contract staff. How do we address this challenge? Long-term we need to increase the pipeline so that we have more workers available to work in our rural communities. And I think programs where you can grow your own workforce at home and people can train in their community and stay in their community, obviously, are the best solutions.
[00:05:20] Dave Northfield: Here’s one from John Q. Murray. Becky, you mentioned workforce initiatives that would allow healthcare students to train in their own communities and go on to work in their own communities. There may not be any bills in the short session, but have you seen any other Oregon bills that would implement this practice?
[00:05:38] Becky Hultberg: I’m not going to speak specifically to this particular practice, but there are some workforce bills in the short session that I think could be consequential. The governor has a workforce proposal in the short session and Rep. Prusak has a proposal specifically related to the nursing workforce. So we’re going to be supporting those, evaluating those, and then moving forward, we’ll be looking at other ways that we can support good public policy to increase the healthcare workforce over the long term. That is what will solve our staffing situation, is, encouraging young people to go into healthcare professions, to train more healthcare professionals, to ensure that we have the infrastructure to train them. And that will be our focus moving forward.
[00:06:12] John Q: Rep. Prusak introduced herself earlier this year.
[00:06:15] Rep. Rachel Prusak: I am the State Representative for House District 37. I am chair of the House Health Care Committee, as you mentioned.
[00:06:21] But what I think most important what guides my work within the committee is that I have been a nurse on the front lines for over two decades and a family nurse practitioner for over a decade. And over the last two years being on the front lines of this pandemic— I specialize in primary care, palliative care and hospice care, and my patients are homebound, so they reside in long-term care adult care homes and in their own home.—so I really saw up close and personal everything that occurred during this pandemic.
[00:06:51] John Q: Rep. Prusak opened her committee hearing Jan. 13.
[00:06:55] Rep. Rachel Prusak: Over the interim, I convened a work group to discuss Oregon’s nursing workforce shortage and consider possible solutions. Over the course of several meetings, the coalition identified multiple overarching problems contributing to the nursing shortage, and while we cannot possibly address all potential solutions in the short session, several of the short-term solutions can be and must be addressed now.
[00:07:21] There are inadequate clinical placement sites for student nurses delaying their graduation and entry into the workforce. There’s a shortage of preceptors for nursing students, making student clinical placement difficult. And while there are many solutions to this extensive problem, including training more nurses, this policy will immediately help nurses and nursing students by developing a nursing student program with licensure requirements.
[00:07:45] Another top issue is that our non prescribing clinicians are not included in the Oregon wellness program. During the pandemic they have suffered mental health issues while not having access to adequate support services. This policy will appropriate money… extending the Oregon Wellness Program to cover all nurses.
[00:08:04] Another issue is that our emergency nursing licensure is restrictive. So this policy will extend emergency licensure requirements relating to staffing shortages from 30 days to 90 days. And for all types of nursing, not just critical care.
[00:08:19] Oregon is the only state where the nursing board is prohibited from accepting payments from licensure, from anyone other than the applicant, third party payers. So this policy will make a small change to allow for payment of nursing license related fees by persons other than the applicant.
[00:08:34] We will require the Oregon healthcare workforce committee to convene a work group, To work on the long-term solutions. addressing staffing shortages in nursing fields. And with that, I’d like to invite up Andi Easton.
[00:08:49] Andi Easton: I’m Andi Easton on behalf of the Oregon Association of Hospitals and Health Systems. And I’m here today to share our support to LC 271. …
[00:08:59] Our workforce is facing the hardest phase of this pandemic. Patients that no longer are needed at that hospital level of care have no place to go and are staying longer in our facilities. Currently, there are more than 600 patients awaiting discharge to a post-acute care setting. At the same time, hospitals are boarding more than 200 patients in our emergency rooms as they await for a hospital bed.
[00:09:26] This is creating a new level of stress on our healthcare providers. With no recovery time for our healthcare heroes over the last two years, many are experiencing frustration, anger, burnout, and trauma.
[00:09:40] John Q: The short session begins February 1. Entering year three of our global public health emergency, many thanks to our local health care heroes.